People suffering with chronic pain and illness can naturally spend a lot of time thinking about how their pain is affecting their lives, every single part of their lives. Pain can make you feel like you are now useless, worthless.
It can tear apart families and bonds we thought were forever, cost careers, friendships and freedom. The irony is that the more you believe these frightening, catastrophic things are going to happen, the more anxious you become and the more your pain goes up.
Counselling and Pain Psychology
Adding a psychological approach to your pain management tool kit can help you develop coping skills that will decrease anxiety, depression, anger and guilt – all of which help to decrease pain and increase your ability to live with pain.
Everyone who lives with pain on a day-to-day basis knows how much stress can affect our pain levels. Depression, anger and anxiety too can all affect our pain in negative ways.
Although a therapist can help you release repetitive or unhelpful thoughts, not everyone is able to utilise their services. So in the interest of making you feel better, here is a guide to using the very techniques a pain psychologist would suggest to help you reduce the negative thinking that so naturally comes with chronic pain and illness.
Do not be hard on yourself. No one who has to deal with the lunacy that is CRPS/RSD or the barrage of symptoms that is fibromyalgia and CFS, can be blamed for negative thoughts.
We’re human. Being ill and never feeling comfortable or well can strain even the most balanced of souls. Instead of blaming yourself, your pain condition or past events, focus on things that help you heal, cope and live again. Your life can be better, I hope this offering helps you cope.
If you are able to see a professional, either in person or via Skype if you are housebound or currently bedridden, then do so. The investment could mean you cope better and also know how to handle flares and crisis.
They are likely to recommend combining medicine, gentle therapies and psychotherapy. Realising that you have someone who can listen and advice you can be such a relief for many chronic pain patients who are struggling to manage the endless symptoms and challenges.
Cognitive behavioural therapy (CBT)
Cognitive behavioural therapy (CBT) is a bit of a life-saver at times. It may take some dedication to learn initially but the knowledge it brings may frequently be a saviour of sorts. CBT aims to enhance your ability to cope by changing dysfunctional thinking and behaviour, which is exceptionally useful when negative thoughts and depression start to rule your mind.
Recent studies show this form of therapy is a particularly helpful component of chronic pain management and I can personally attest to its virtues. Psychologists say that CBT helps chronic pain patients by ending the downward spiral of negative thinking that worsens pain and coping.
People suffering with chronic pain and illness can spend a lot of time thinking about how their pain and its penetrative effects. No part of our lives is unaffected by our pain and complicated condition. So it is natural to focus on this but the irony is that the more you believe these frightening, catastrophic things are going to happen, the more anxious you become and the more your pain goes up.
Yet using CBT techniques can stop these thoughts in their tracks and actually help reduce your pain. Even if you have lived with your pain condition for many years, these techniques are worth learning and can help you release pent up emotions and cope during flare-ups or set-backs too.
Thinking negatively about their pain, growing concerned, anxious, or pessimistic, though a natural and very human response, these thoughts can actually increase pain levels, so psychologists and therapists work with patients to reframe some of the negative thoughts surrounding their pain.
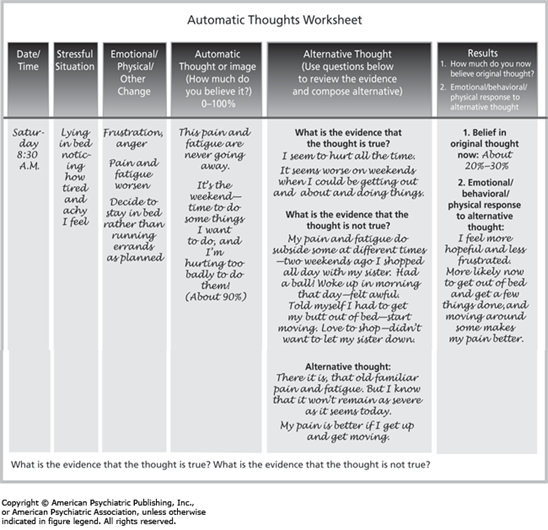
An example of one of the many CBT tools and techniques is illustrated below, with this ‘Thoughts Diary’, it shows the automatic thoughts in a given situation, questions the evidence as to whether the thought is true, offers alternative thoughts and finally gages both belief in the original thought and your emotional and physical response to this newly interpreted thinking:
Cognitive-behavioural therapy helps you change the way you think about the pain so that your body and mind respond better when you have episodes of increased pain, such as a flare-up or breakthrough pain. Therapy focuses on changing your thoughts about illness and then helping you adopt positive ways of coping with illness. For cognitive-behavioural therapy to be most effective, work together with your psychologist or counsellor toward common goals.
For a blank CBT Thought Record sheet, click here.
Another CBT technique involves writing down a negative thought on one side of a card. On the other side, write a rational comeback to that thought. When a destructive thought comes along, patients can reach for their card and repeat the coping statement to themselves. Almost everyone can come up with something kind to say to a friend who is upset – be your own best friend and be mindful of your internal chatter, veering away from any ‘catastrophizing’ thoughts, such as those illustrated in the table below:
| Chronic Pain Situation | Negative Thought | Coping Thought |
| Pain flare | “This pain will never end.” | “I’ve had bad flare-ups before and know I can get through this.” |
| Pain flare | “Why am I being punished?” | “There are millions of people in pain. I am not alone, and I am not being singled out.” |
| Missing a day of work because of pain or having to stop work altogether | “I won’t be able to support myself/family.” | “Missing one day does not mean that I can’t return to work””My health is the biggest priority, I hope to return to work one day but if I cannot I must accept this change in my life.” |
| Frustration at not being able to do what you used to | “I hate asking for help. I should be able to do this on my own.” | “I will be better off in the long run if I ask for help with certain tasks. Most people are happy to lend a hand.” |
| Trip to a cafe with friends | “If I go out with my friends and I can’t keep up, it will spoil it for everyone else…I hate having to depend on them and have to ask them to push my wheelchair” | “If I plan ahead, take some breaks, and let my friends know I am going to do this, I can keep up and still enjoy being with them.” |
| Can’t tolerate the drive to a friend’s wedding | “My pain interferes with everything in life.” | “I may need to change my plans and miss out on many celebrations but I still love my friends and they still love me; I hope that they understand.””If I plan ahead and modify how I do this (e.g. enlist the help of another if you do not have a carer; break the drive up with rest breaks and arrive at a hotel a day early to pace yourself). I can still do some things I enjoy if I pace myself.” |
| Unable to do household chores | “This place is such a mess and I can do nothing about it. I am worthless.” | “There are lots of things I do for my family and others. Housework does not define my worth.” |
| When children visit | “I can’t even lift my own child/my friend’s child/my grandchild… She probably thinks I don’t love her anymore.” | “There are many ways to show and express love; communicating and saying how much I love them will be heard and I’m so happy to have them in my life.” |
Unhealthy Thinking Patterns in CBT
Read the following unhealthy thinking patterns to see if you recognise them in order to remedy and change your perspective to something more healing and positive:
All-or-None Thinking – Definition: Looking at a situation as either black or white; thinking that there are only two possible outcomes to a situation
Example: “If I am not a complete success at my job, then I am a total failure.”
Catastrophising – Definition: Expecting the worse to happen without considering other alternative outcomes that are more likely to happen
Example: “I know that I will be so anxious that I will bomb this test and fail the course.”
Labelling – Definition: Defining yourself or others in a rigid way that doesn’t allow for more favourable evaluations
Example: “I am a total loser.”
Discounting the Positive – Definition: Looking past and ignoring positive experiences; viewing positive experiences or outcomes as simply being due to chance
Example: “I got that job out of luck, not because I was qualified.”
Mind Reading – Definition: Thinking that you know what others are thinking
Example: “I just know that my therapist thinks I am a waste of his time.”
Personalisation – Definition: Evaluating other people’s behaviour as being the result of something you did
Example: “She wasn’t very polite toward me because I must have done something to upset her.”
Emotional Reasoning – Definition: Believing something is true because it feels that way
Example: “I must have failed that test because I feel so bad about my performance.”
To benefit from these technique, ideally see a therapist trained in using CBT specifically for chronic pain, who will help you create a list of coping thoughts relevant to your personal situations and everything you are having difficulty dealing with. The goal is to reframe the thoughts and change the pattern.
By identifying and changing negative thought patterns and teaching patients to be aware of the automatic thought patterns that occur have when the pain worsens or indeed, from day to day life with chronic pain.
Acceptance and Commitment Therapy or ACT
A newer form of CBT, called Acceptance and Commitment Therapy or ACT (typically pronounced as an acronym, not an initialism) is a cognitive–behavioural model of psychotherapy. ACT uses acceptance and mindfulness strategies mixed in different ways with commitment and behaviour-change strategies, to increase psychological flexibility and coping skills. A wonderful introduction and guide to ACT is a book called ‘The Happiness Trap (Based on ACT: A revolutionary mindfulness-based programme for overcoming stress, anxiety and depression’ By Russ Harris, follow this link to buy a copy from Amazon.
Sign-up and receive a free flare-up toolkit and regular posts and tips on living – and coping – with severe pain and chronic illness ♥
[avatar user=”jomalby” size=”thumbnail” link=”www.princessinthetower.org” target=”_blank”] Gentle hugs x[/avatar]

have fibromyalgia and degenerative dic disease and osteo arthritis
Excellent article! Thank you for the very clear advice. I’ve also learned that CBT is one of the most effective techniques for pain management but also for anxiety and depression.
Pleasure, Elviira, so pleased you enjoyed it. Completely agree, CBT is one of the finest tools I’ve come across to help, particularly with the emotional side of living with pain, and especially for anxiety and depression. I’ve also enjoyed ACT or acceptance and commitment therapy, from which I’ve slipped a few tools into posts but planning to go deeper in a post of its own. Wishing you many spoons and far better days. ♥ x
I have Fbromyalgia and don’t constantly think about the pain. I feel it and go through the moment.
I’m alergic to morphine and refuse to use diclofenac (which is really bad for you), so here in the Netherlands (where I live) I don’t get any other medicine from my doctor. They still don’t see it as a real disease here. So when my pain is too bad I’ll take ibuprofen (only when I can’t handle it), it’s the only thing I use. I’m also glad I have a high pain tolerance so the pain don’t bother my as much. I hated de numbness I felt while using medicins like zaldiar. I even had blackouts while using zaldiar and being tired isn’t fun either. For me it’s worse because it makes me feel old.
There is a Small Fiber Neuropathy clinic in the Netherlands…. 50% of Fauxbromyalgia as I lhave coined it, have SFN which rules out a fibromyalgia diagnosis. Here in USA but probably where you are too, only Therapath Labs offers the two easy, skin punch biopsies…. Epdermal Nerve Fiber Density and Sweat Gland Nerve Fiber Density. My ENFD was negative which impeded diagnosis since two neurologists thought I had less sweat glands. The lab said the SVNFD test is a better and earlier indicator of SFN & 18% of patients will only be + on SGNFD and negative on ENFD. A neurologist will take 2-3 punch samples from your worst leg….some do arms, too,, in office then you go home….don’t even recall any pain after lidocaine wore off. Not to be confused with a sural Nerve biopsy which is a big deal & leaves a permanent deficit or nerve injury although small…..no thanks!
I have excellent coping,, already. Less neuropathic pain (& for all my other chronic pain) from Norco & methadone. They were afraid to increase Fentanyl over 150 mcg every 48 hours, but it also helped. Cannot tolerate most meds.
Look up Palmitoylethanolamide…..I almost ordered it from Netherlands, since that SFN clinic tested it but I found an American company.. The one in Netherlands has both capsules & topical so may still order. It helps my pain, actually best results yet so for the first time since SFN began to ramp up (2011) I no longer am constantly aware of my legs & need to distract myself! My meds have NEVER been titrated to effect so have been in agony for over a decade & my pain MD fired me over the new SFN pains, but that’s another story!!! The methadone 20 mg three x a day was great comparatively but only made the SFN pain tolerable so I no longer had to stomp & slap my legs, like I did for 2 years on Fentanyl. Getting adequate pain medication here is impossible due to Fascist Government agencies preventing Physicians from prescribing according to their textbooks, PDR’s & journal s so I am always looking for natural help. Palmitoylethanolamide is a fatty acid which has good studies to show safety & effectiveness…. I cannot benefit by telling you this….just please look into it. My new pain MD said for me to continue and increase till no more improvements felt then can try to decrease to a maintenance dose. I started at two 350 mg capsules three times a day, with a fat (heavy cream/half & half in morning coffee, afternoon supplements with fat like vitamin E, Lutien, garlic coconut oil) & dinner when I usually eat, anyway)….took me two weeks, some take 5. Most take a few days. Low carb/grain-free always decreases my Fauxbromyalgia’ pain , too so looking forward to combining with that. 600mg alpha lipoic acid boosts PEA, also 3 times a day. Intractable pain needs every weapon we can use! Medication, natural, Physical Therapy, yoga, CBT & spirituality & supportive family & friends. So, target therapeutic dose range for neuropathic pain is 80 to 120 mg methadone & with the PEA my 60 mg fees like 80 & I have decreased SFN pains in both shins and a smart area!