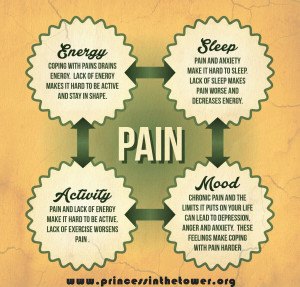
When you have constant pain, it’s no secret that trying to get to sleep – and stay asleep – is far from simple. Sometimes we’re wired from the pain all night, resigning ourselves to the endless monotony of longing to escape both physical agony and find slumber. Other times we may be blessed enough to fall asleep initially but then wake, entirely unable to return to that place. Before you despair at the idea of never feeling rested again, this post focuses on ways to optimise your chances of sleep.
Pain and Sleep
Pain is of course, difficult to sleep with. Especially when in the quiet of the night it seems to grow all the more fervent. Many pain patients, especially those with severe pain such as with CRPS/RSD or neuropathic pain, wake many times in the night to what feels like even worse pain than when sleeping, causing further distress and difficulty returning to sleep.
Other chronic pain patients including many I know who live with fibromyalgia, have cycles of three or four days, where only twice a week can they sleep more than a few hours if at all, or they find themselves entirely sleep deprived for many days only to sleep for an extended period, as if the body itself is reclaiming sleep.
In one study conducted by Felix Naughton and his colleagues, poor sleep quality made those with chronic pain feel more depressed and also tended to make their pain feel more intense. Another study on patients with fibromyalgia, Dr. Nancy Hamilton and her colleagues found that poor sleep had a cumulative effect on negative emotions, also interfering with emotional recovery on days in which the person experienced a high number of stressful, negative events, all of which everyone with pain knows makes their pain worse.
Although there have been no epidemiologic studies conducted on sleep disorders in people who have CRPS, the clinical observations of R. Norman Harden, MD, Clinical Co-chair of the RSDSA Scientific Advisory Committee and Director at the Center for Pain Studies, Chicago, are that at least 75% of people with CRPS, possibly as many as 90%, have some sort of sleep disorder. “Pain is, of course, the main culprit for those who have difficulty falling asleep and for those who have difficulty staying asleep,” says Dr Harden.
“At bedtime, the mind starts to relax, and since there are no distractions the mind naturally focuses on pain. Early morning awakening may occur if a person rolls onto the affected limb and is awakened by pain. Treating the sleep disorder is critical, not only because people who sleep well feel better, have more energy, and are in a better mood, but sleep is critical to the bodys recuperation, repair and healing, especially with chronic disease.” Read more here and also see: RSDSA :: Reflex Sympathetic Dystrophy Syndrome Association.
What You Can Do: Tips to Help You Sleep
Staring at the Clock
You may find that simply getting through the day has washed you out completely and that sleeping, initially isn’t the problem but that very soon you wake again, or the pain wakes you up, and so again you lie there in excruciating pain unable even to sleep and escape it. Similarly, when unable to sleep, if you find yourself staring at the clock as the night ticks away and fretting about how little sleep you really have, this too can result in a vicious circle of sleep deprivation.
“These are all perfectly natural responses – but they only make you more anxious and your insomnia worse. Take control of your thoughts so that you are not making yourself feel more anxious than you need to,” says says pain psychologist, Linda Reuhlman. It’s natural to respond to sleep difficulties with concern but this can only worsen the cycle.
If you lie in bed worrying about how you will be able to function in the morning or cope with increased symptoms and pain in the day, or if you become anxious before trying to sleep as you are so used, as used as anyone can be, to almost no sleep at all, both of these reactions can lead to increased insomnia.
“You may say you can’t fall asleep because you are in pain and then, your lack of sleep makes you hurt more, you may feel your mood worsening, you may feel able to do less, feel bad about that, then sleep less….and the cycle continues,” says Linda Reuhlman. “People with insomnia often get caught up in thoughts that make their insomnia worse.”
For psychology techniques to reduce negative or unhelpful thinking, visit How to Use Pain Psychology Techniques to Reduce Anxiety, Depression, Anger and Guilt, you may also enjoy: Living with Pain: Sleep Quality, Depression, Pain and Disability.
Changing habits that disrupt sleep
Certain habits are so deeply ingrained in our lives that you may overlook them as a possible reason for your insomnia and other sleep problems are worsening, outside of the challenge that is to sleep when in so much pain, of course. “One of the most important recommendations is to go to bed and get up at the same time each day – yes, that means weekends and vacations too. This helps to maintain a regular sleep cycle in your brain,” says Reuhlman.
Cut the Cup o’ Joe
Maybe you drink excessive amounts of coffee during the day, making it harder to fall asleep later. Some stop caffeine after about 2pm, others can have a cup at 4pm and still manage to sleep. Find what works for you and stick to it.
“Don’t lay in bed tossing and turning. If you haven’t fallen asleep after 20-30 minutes, do something for a short time, then try again,” says Reuhlman. “Don’t use alcohol to help you sleep. It may help a bit at first, but it will lead to disrupted, non-refreshing sleep…and over time you will need more and more to get to sleep.”
Late Night Television
Perhaps you’ve never made the connection between your late-night TV watching or lingering on the internet and your sleep problems but your brain needs to wind down, relax and calm. Preparing your brain to sleep is crucial. One key to this is to spend the last hour before sleep doing entirely passive, non-stiulating activity. So for example, reading by a low light is ideal.
Keep a Sleep Diary
Keeping a sleep diary can be a helpful way to pinpoint any habits or routines that could be worsening or contributing to your insomnia. Simply keep a record of what you did each day, much like when you are pacing your activity to minimise your chronic pain levels, and write your daytime activities, habits, sleep routine, times you managed to sleep and the insomnia.
Preparing your brain for sleep
- Increasing light exposure during the day.
- Taking breaks outside in sunlight if possible and open blinds and curtains during the day.
- Limit artificial light at night. Some sleep experts suggest using a low watt light for the last hour before you try to sleep.
- To boost melatonin production, use low-wattage bulbs, cover windows and electrical displays in your bedroom, avoid bright light and turn off television and computer screens at least one hour before bed.
- If you can’t make your bedroom dark enough, try using an eye mask.
- Using techniques to calm and relax you before you try to sleep help many pain patients have more sleep. Try this restorative body scan technique an hour before you want to rest, or perhaps you’ll find that these 3 Natural Ways to Reduce and Manage Your Pain help you get to sleep too.
Pain Management
As pain and complicated conditions that cause a lot of chronic pain require a multi-disciplinary approach, by ensuring you learn all you can about chronic pain and pain management, you will help both your ability to cope and your symptoms, including sleep and insomnia.
“A sleep disorder caused by pain requires a multi-disciplinary approach, you not only need the advice of a physician who specializes in pain management, but you need access to psychologists who are trained in behavioural medicine,” says Jackie Randa, a physical therapist who owns Back on Track in Barstow.
“Pain management, in my opinion, has been relegated to the position of “last chance” medicine. Folks are not referred to these valuable centers until their doctors decide there’s nothing else that can be done. Pain management should be part of your care all along if you have a condition which will cause significant pain.
“Behavioural medicine can be quite effective in helping not only to improve your quality of sleep but can help you manage your pain more effectively. There are a number of effective sleep medications which might help you get some rest in the mean time, but for a long term solution, behavioural medicine is best. The lessons you learn will last your entire lifetime without adverse affects.”
Adopting new habits to help you sleep
- Noise, light, and heat can interfere with sleep. Make sure your bedroom is quiet, dark, and you warm enough but the room not too warm as most people sleep better in a cooler atmosphere. The ideal temperature according to the Sleep Foundation, is 65 degrees fahrenheit. For more on finding the optimum temperature for sleeping, read this.
- You may find that keeping the room fairly cool but using a timed heat pad/mat offers useful pain-relief and helps you sleep. One company I love to bits is Gentle Heat who offer a range of great products, including a heat wrap that you can also wear during the day if heat is something that helps you. I know it truly helps me, take a peek here: Gentle Heat.
- Try using a sound machine or earplugs to mask outside noise, you may enjoy listening to the rain, ocean or rainforest, all of which you can find on apps or using a sound machine. For more information on how noise and sounds effect sleep, and what to choose for you personally, visit the Sleep Foundation’s page on sound here.
- An open window to keep the room fresh, and blackout curtains or an eye mask to block out light.
- Stick to a regular sleep schedule. This is important as it supports your biological clock when you always go bed and get up at the same time every day, including weekends. This can help you get back in a regular sleep rhythm, which in turn helps your body sleep more regularly.
- Manage your fatigue with short naps. Napping during the day can make it more difficult to sleep at night for many people but for those with severe chronic pain and fatigue, little naps are often what enable us to make it through the day. A 20-minute nap can be ideal. If you feel like you have to take a nap, do limit it to 30 minutes (before 3 p.m. if you find that it inhibits sleep at night time) as after this, you will fall into a deeper sleep which will not be energising but make you feel even more tired. The Sleep Foundation has more info on napping and what the optimum way to do it here.
- Avoid stimulating activity and stressful situations before bedtime. This includes vigorous exercise; big discussions or arguments; and TV, computer, or video game use.
- Limit caffeine, alcohol, and nicotine. Stop drinking caffeinated beverages at least 8 hours before bed. Avoid drinking in the evening. While alcohol can make you feel sleepy, it interferes with the quality of your sleep. Quit smoking or avoid it at night, as nicotine is a stimulant.
- If you are flared-up, try these pain-reducing techniques for severe pain.
Letting Go of Anxiety When You Can’t Sleep
The more trouble you have with sleep, the more it starts to invade your thoughts. You may dread going to sleep because you just know that you’re going to toss and turn for hours or be up at 2 a.m. again. Perhaps you’re worried because you have a big day tomorrow or a vital medical appointment and you just cannot relax or even come close to calm.
Natural Treatments for Insomnia
- Ten Natural Sleep Tips – Describes ten natural remedies for insomnia, including lifestyle changes, herbal supplements, and relaxation strategies. (Dr. Weil)
- Insomnia Treatment: Cognitive Behavioral Therapy Instead of Sleeping Pills – Your attitudes about sleep and certain behaviors are often the root cause of insomnia. (The Mayo Clinic)
- CBT for Insomnia Program – Online, interactive treatment program for insomnia from sleep doctor Gregg Jacobs. A Harvard Medical School study found this program to be more effective than Ambien. (cbtforinsomnia.com)
- Insomnia Treatment – Covers a wide range of insomnia treatments, including sleep restriction, stimulus control, cognitive behavioral therapy, and relaxation techniques. (QualityHealth.com)
- Sleep Restriction Therapy: When Nothing Else Works – Step-by-step guide to sleep restriction therapy, an effective insomnia treatment that involves limiting time spent in bed. (Talk About Sleep)
- Cognitive Behavioral Therapy for Insomnia – Describes how cognitive behavioral therapy works treating insomnia, and provides a case study as an example. (National Sleep Foundation)
- Melatonin and Sleep – Discussion of melatonin’s use in the treatment of insomnia and how it may help when you can’t sleep. (National Sleep Foundation)
- Valerian – A review of the use of valerian for treating insomnia and other sleep disorders. (Office of Dietary Supplements, National Institutes of Health)
- This Facebook group is wonderful for chronic pain patients: Chronic Pain Information Group – it’s run with the unique mandate: for pain information first and conversation second.
You may also find these links useful:
- Mattress Guidelines for SleepComfort
- Practicing Good Sleep Hygiene
- Chronic Pain and Insomnia: Breaking the Cycle
- Sleep Aids for People with Chronic Pain
- Pillow Support and Comfort
- Review of Adjustable BedsBest Mattress for Low Back Pain
- Insomnia Medications – Non-Prescription
- Chronic Pain Management: Improve Your Sleep
- When Pain Interrupts Your Sleep
Information About Insomnia:
- What is Insomnia? – A series of articles covering different types of insomnia, the causes of transient and chronic insomnia, self-help cures, and professional treatment. (University of Maryland Medical Center).
- Facts About Insomnia (PDF) – Fact sheet describes the symptoms and common causes of insomnia, as well as proven treatments and cures. (National Institutes of Health).
- Can’t Sleep? What to Know About Insomnia – An overview of insomnia including common causes, signs, symptoms, and what to do (National Sleep Foundation).
- Insomnia – Discusses insomnia symptoms, types, causes, and treatments, including what you can do to stop sleepless nights. (University of Cambridge).
[avatar user=”jomalby” size=”medium”]Gentle hugs x[/avatar]









My wife has rsd. . Its crippled our lives together for years now. She’s tried everything. Biggest problem is sleeping for her. I’m not sure how much longer she can deal with it..
My parent deals with the same problem, and I’m unsure how she’ll be able to cope the longer this goes on.
All the best to the both of you,
I didn’t sleep at all last night. Bad arthritis in right hip. Terrible right leg pain. I took some benedryl and nyquil with no relief. Florida doctors don’t really care. I’m starting to hate everyday that goes by. Thanks for letting me vent.