Chronic pain isn’t just a condition, it’s a full time job. From CRPS to fibromyalgia to old injuries that just refused to heal, unless you take your pain into account during every activity, every moment whether resting or recovering, the pain will pay you back that night and/or over the next day, days or even weeks. Managing pain is a bit of an artform. Always be mindful of pacing and resting as it is one major key to YOU being in control of your pain – as much as possible – and not the other way around.
The Key to effective pain management pivots largely on your attitude to the pain, see Using Pain Psychology to Help You Live and Cope with Pain. Negative thoughts can stop you from taking positive action. It’s hard to help yourself when you feel depressed or filled with negative feelings. Recognising the effects of situations on our feelings as well as our own reactions and thoughts can help you cope.
Although there is a lot of variation between chronic pain patients the management and treatment can be helped in many similar ways no matter what caused the pain you have now. Relaxation techniques, pain pacing, mindful movement, psychological techniques/overcoming negative self-talk and reducing depression, complimentary medicine and healthy eating (treats are good too, don’t deprive yourself), can all help you live and cope with pain.
Fluctuating Symptoms and Unpredictable Pain
Just as our symptoms vary unpredictably, our ability to cope with our pain ebbs and flows too. It can be incredibly hard to keep going some days but this site is here to help make living with chronic illness and pain more manageable, rejoicing with you on the good days and support you through the bad.
From The Princess in the Tower Facebook community:
“No one understands. I am always at the mercy of this monster that no one can see.”
“I just wish they’d believe me so I didn’t have that extra stress on top of trying to cope with the pain.”
“People get annoyed at how unpredictable my pain is but they don’t have to feel it too. It is far more annoying for us who live with it. You can’t ever tell from one day to the next how bad it would be. Only that it will be.”
What is Pain?
Knowing how our bodies experience pain can help you manage it. People tend to associate the pain they feel with the body part (or parts) that are affected, that is they associate what’s going on in their arm or their back as pain ‘out there in the body’ but it’s actually a process called nociception: electrochemical signals generated in our body in response to injury that get transmitted along nerve fibres to our spinal cord and up to our brain, where they’re processed and become the experience of pain. It is your brain and nervous system.
For example, if you injure your arm, that’s not pain in your arm, that’s nociception. Nociceptors are special pain receptors that activate whenever there has been an injury, or even a potential injury, such as breaking the skin or causing a large indentation, if the tissues in your arm become compressed enough, it causes the nociceptors to fire off a response. This impulse travels through the nerve into the spinal cord, and eventually all the way to your brain and it all happens within fractions of a second.
Pain can be an acute event, which signals there is harm and you need to get away from it. In the above scenario, after your arm has healed, the pain sensations should stop because the nociceptors no longer detect any tissue damage or potential injury. This is called acute pain. Acute pain does not persist after the initial injury has healed.
Sometimes, however, pain receptors continue to fire… This can be caused by a disease or condition that continuously causes damage, such as osteoporosis for example, or – as is the case with RSD/CRPS and Fibromyalgia – sometimes, even in the absence of tissue damage, nociceptors continue to fire.
There may no longer be a physical cause of pain, but the pain response is the same. This makes chronic pain difficult to pin down and even more difficult to treat. Unfortunately, when pain becomes chronic, when it’s present for long periods of time even after the tissue has healed, we can still have this perception of pain even though there is no obvious tissue damage or injury.
The pain actually causes rewiring and alterations in our nervous system called neuroplasticity, where the brain appears to ‘learn’ to repeat sending pain signals, despite the original trauma or trigger to have healed a great deal of time earlier. The brain controls the nerves and tell them how sensitive to be. When anxious, the brain might request “more information” from the peripheral nerves so they produce more signals in response to stimuli that usually does not cause physical pain or it may do the exact opposite.
Messages about pain do not just go up to the brain, they also go down. It’s this two-way functionality that is the principal difference between former beliefs about pain and modern pain science. There is now extensive evidence that the peripheral nerves can physically and chemically change.
This may be in response to these brain signals, tissue conditions, or both. This isn’t just turning the volume up on your pain but changing the entire equipment and changing the signal before it even gets to the “amplifier.” That is, we only feel what our brains allow us to feel.
Even “loud” sensory messages can be filtered down to almost nothing by the central nervous system (as detail in Lorimer Moseley’s story) or, conversely, “quiet” sensory messages can be greatly amplified, worsening the intensity of the pain you now feel. The quality and intensity of the pain experience is the result of all these neurological filters. To learn more about this process, visit Central Sensitization.
Also see: Central Sensitization: A Generator of Pain Hypersensitivity by Central Neural Plasticity.
Chronic Verses Acute Pain

It’s vital to realise that there are huge differences between acute pain and chronic pain. You will get very different results if you treat them the same way. Acute pain is the byproduct of tissue injury and damage. It is the pain we feel when bones are broken or tendons are torn.
Chronic pain, on the other hand, is the disease. It is a complex equation of physical, emotional, cognitive, genetic and environmental factors that come together with the end result that leaves us hurting in some way, day after day.
It is in the chronic pain setting that the neural plastic properties of the brain can lead to maladaptive changes in the brain’s wiring that both make us feel lousy and change our behaviors into seemingly a different person. True healing requires re-wiring these adverse changes into something more positive and less taxing to the brain.
Pain neurology cannot be manipulated by longing for it to stop, as much as many people may have told you “not to think about the pain”. The brain may powerfully control our experience of painful experiences but you don’t control your brain. Consciousness and “mind” are by-products of brain function and physiological state. It’s not your opinion of sensory signals that counts, it’s what your brain thinks of it — and that occurs quite independently of consciousness and self-awareness.
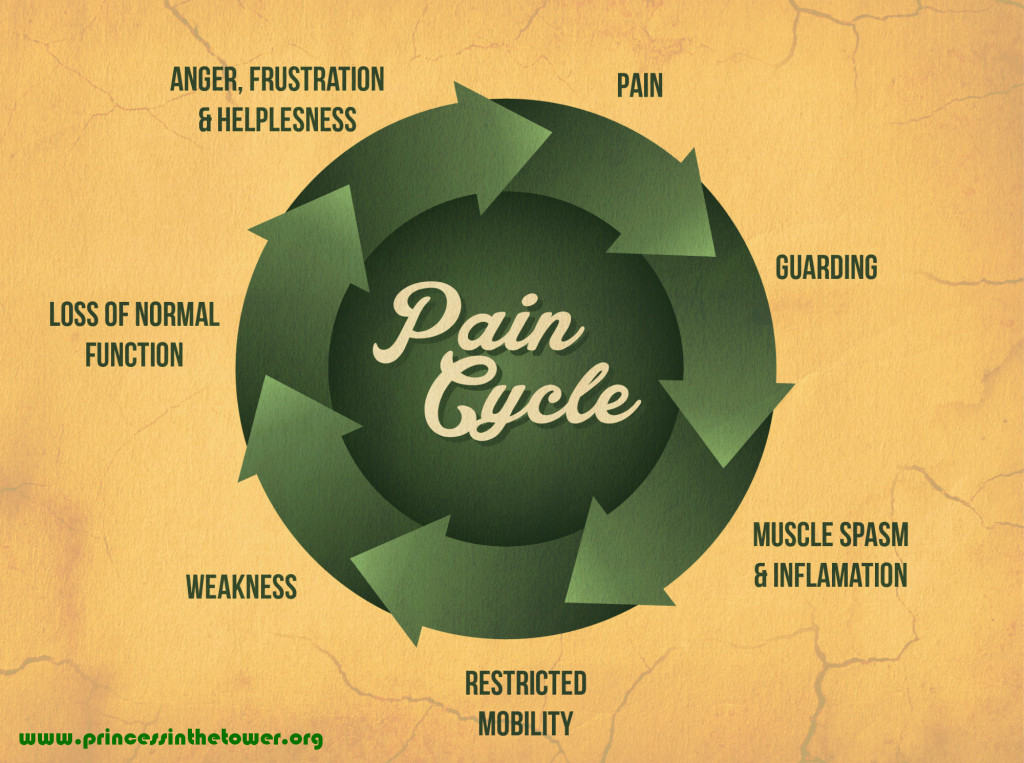
The nervous system is a complex electrical network in the spinal cord and brain which increases or blocks the transmission of pain. In chronic pain the pain gates – which let the pain signals through when it is open and blocks pain signals when closed – will not close and as a result pain behaves like an over-sensitive car alarm.
It reacts to what should be harmless stimuli, and behaves as if stuck on the ‘on’ position, continuously sending pain signals long after the injury or original causes should have healed. It’s important to learn how to minimise the pain and help calm your over-active nervous system using techniques found herein.
Managing Chronic Pain
It’s up to your medical professionals to show you how to best manage that pain yet frequently those with chronic, intractable pain are left to work out this mysterious management on their own. Fortunately, the internet is now rich with websites that can offer you support and information. If you are careful to check the sources, it can be very useful. Though the cream of the crop will all be regularly published here.
Using medication, physical and occupational therapy, or mind/body/spirit approaches, all of these show significant benefit in reducing patients’ pain and helping them improve quality of life and physical functioning. In the spirit of being a proactive patient, playing a part in your own healing, the best-known pain management techniques are outlined below. Learn more about what pain is this excellent talk with Lorimer Moseley:
Once you have been plagued by chronic pain for many years it becomes an old adage but a true one that if you don’t control the pain, it will control you. Learning pain management techniques, either through a pain clinic management program or through a pain psychologist/pain specialist will give you at least some of your valuable life back. Sadly, not everyone makes it to a pain clinic and suffer needlessly for years at a time.
Pacing to Manage Your Pain
The first rule of chronic pain management is pacing. Finding the exact amount of activity you can do without causing a flare-up of symptoms is almost an art form. The trick is to work out your time limits on activities such as sitting, standing, walking etc., and how long you can do each activity on a good day and how long you can do them on a bad day.
By limiting yourself to always stopping after the length of time you could do the activity on a bad day, you won’t push yourself to do more on a good day and consequently suffering for it the following day. Pacing is a concept that pain specialists and pain psychologists instruct every client who is suffering from chronic pain.

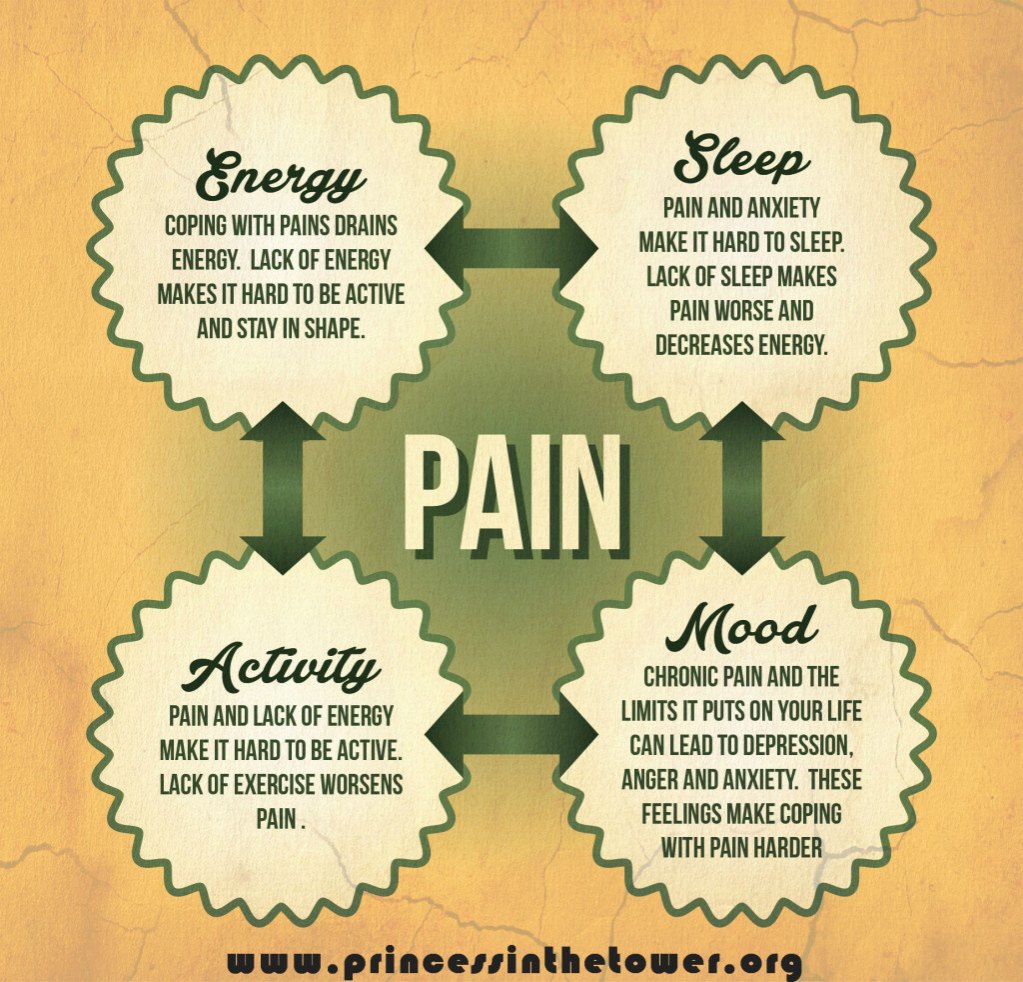
Many chronic pain sufferers are naturally far less active than they used to be and as a result, you may have noticed yourself trapped in a cycle of ‘boom and bust’ with activity and exercise.
An example of this is someone who wakes up one day and feel they are having a ‘good day’ and so decide to catch up on things while pain levels are manageable. Later that evening the symptoms are flared-up again, resulting in extended rest and ‘bad days’. Eventually it settles and the pattern is repeated again when they feel a bit better.
Another pacing problem is around those day to day chores that need to be done. These are the normal Jobs at work and home that build up around us. If there is a day when you feel better the the temptation is to try and do everything all at once because you don’t know when the next opport
unity will be.
A third approach is the ‘never give in’ attitude. Refusing to let the pain beat you and stop you from doing what you want and need to do. This is when it feels you are at war with your pain and you are not going to let it win; the result is harmful on both a short and long-term basis. With all these ways of approaching activity, it is followed by more pain and for some more inactivity follows as you try and settle it down – the ‘boom and bust’ cycle (see below). Your baseline level of fitness never really improves – if anything it gets worse.
Repeated flare ups of pain lead to more feelings of loss of control, anxiety and isolation as the cycle of chronic pain continues and even worsens. A pacing problem is basing your activity level on how you feel (doing more when you feel good and less when you feel bad). Good pacing involves basing your activity level on pre-set, reasonable goals – not on your level of pain. To remedy a pacing problem, you will need a Pacing Plan that will help you to gradually increase how much you do of an activity, slowly and safely.
It is vital to stop before the pain increases too much and becomes unmanageable and flares-up. This enables you to do more things and have a regular amount of activity each day instead of doing one or two things, being in too much pain to do anything more and being disappointed and in more pain, unable to do anything, possibly for the entire next day. To read more about how to use pacing for pain management click here.
A pacing problem is basing your activity level on how you feel (doing more when you feel good and less when you feel bad). Good pacing involves basing your activity level on pre-set, reasonable goals – not on your level of pain. To remedy a pacing problem, you will need a Pacing Plan that will help you to gradually increase how much you do of an activity, slowly and safely.
Maybe you need 5 minutes rest for every 15 minutes of activity, or an hour’s rest for 10 minutes of activity; the point is to find a reasonable ‘comfort’ level (if while in chronic pain there is such a thing!), while still being active every day possible. Flare-ups can and do happen of their own accord (see this page for dealing with flare-ups and sign-up to the newsletter for a free flare-up tool-kit), however, pacing massively limits the triggers that make so many flare-ups occur.
Remember that setting a timer helps you remember rest periods as it is so easy to continue if you feel you can, thus exceeding your limitations and getting pain payback. Your rest periods are a good time to practice relaxation techniques, sms a friend, listen to music, read a book or meditate. Read more here.
You may discover that you worked productively for a total of two hours, without increasing your pain ‘too much’, whereas, had you pushed yourself to work two hours straight, without a break, you would have increased the pain throughout the evening, night and possibly the next day (depending on your pacing levels), and finished a lot less work.
Cognitive Behavioural Technique (CBT) and Acceptance and Commitment Therapy (ACT)
For psychology techniques to help you cope and manage pain, click here.
Keep a Pain Diary
Another useful pain management tool is to keep a pain diary, not just to help with voicing your thoughts and tackling uncomfortable feelings, but it can also help you pin point pain-flare triggers, such as certain activities or weather changes for example, point out patterns of pain variation, help your doctors understand and help you better, as well as the emotional vent it may provide your feelings to get it all down on paper.
It’s often said that the most important person in any pain management effort is the patient. Every patient living with chronic pain can provide invaluable assistance to their doctors in many ways, and one of the most important is keeping detailed records of the pain they are feeling.
Your doctor will be looking for triggers, stresses, and patterns. The more detailed you can be about the factors that seem to influence your pain, the better. A pain diary or journal can not only help doctors figure out the initial source of your chronic pain, if undiagnosed, but also help them to prescribe the optimum medications, advise of therapies that will better help you manage pain and generally help communication between you and the management of your chronic pain.
As much as your pain diary can help your doctors, it can help you even more. Keeping this record gives you the ability to regain a sense of control over your health, your life, and your pain management. Through the pain diary, you can:
- Figure out pain patterns. You might find that you have pain flare-ups following meals, during certain types of weather, or after physical activity. Knowing these patterns can help you minimise or avoid pain.
- Better understand what works. Those patterns also can give you an idea of what therapies best alleviate your chronic pain.
- Better understand what does not work. You can often learn just as much from what fails as what succeeds.
- Improve your communication with your doctor. You’ll be better able to answer questions about your pain and participate more fully in your pain management if you go to your doctor well-armed with the information you’ve stored in your pain diary.
You don’t have to make a note every time you feel pain; that could be an overwhelming chore that tires you out and, worse, makes you pay too much attention to your pain. Conversely, it is useful to keep a detailed pain diary (for the duration of a week), every three or six months, to help both you and your pain psychologist/specialist and other doctors and health care providers. A simple Pain Diary can be downloaded here.
Pain management experts recommend that people keeping a pain diary make one to three entries a day, at about the same time every day – morning, noon and bedtime, for example – that way, you will fall into the habit of making regular entries and avoid writing only when acute flare-ups occur. Download a three-week Pain Diary here, complete with pain intensity, activities and pain description; as well as a space for morning, afternoon, evening and sleep times.
Develop a Set-back and Flare-up Plan
This is vital in the management of periods of increased pain. For more advice on this and other aspects of flare-ups of pain, sign-up to the Princess in the Tower’s newsletter for a free guide and Flare-Up Toolkit. Also see Coping With Flare-ups of Pain.
Setting Goals and Prioritising
This is a great starting point to build up from; if you have been sedentary for a long time, you’ll have seemingly microscopic pacing limitations but even by sticking to these (see ‘Pacing’ above), it is in your interest to set goals but always be flexible and never scould yourself if you do not manage to meet them.
Make a list of three things that you would like to achieve, even if they are as simple as ‘make my own cup of tea’ as – for many – this could be huge. Other goals, like ‘having a friend visit’ will have to be planned around, i.e. resting and taking medication before, pacing yourself during and stopping before the pain escalates to ridiculous levels is vital pain management (and your friends and other loved-ones need to understand this).
Obviously everyones’ limitations vary so adhering to the above advice and in turn deciding what you will achieve each day, while aiming to keep the same level of activity up for each day is all positive strategy. The idea of planning your activities and planning a rest break before your pain forces you to stop is a key technique of pacing and is sometimes called ‘working to schedule’ – this is in contrast to working to tolerance.
When you work to tolerance, you push yourself to your limit. Over time you will find your good days becoming a thing of the past as the ‘boom bust cycle’ repeats itself. This can be remedied by taking things very slowly and systematically planning activity and rest; by planning and sticking to it, you are in more control of your pain.
Mindful Movement
Although it may feel like it does because of the increase in pain, gentle movement will not cause physical damage and can actually help combat the maladaptive neuroplasticity from the chronic pain (that perpetuates the problem), also strengthens weak and deconditioned muscles and also increases mobility and lessens pain. If I miss my physio therapy and yoga, the pain is far worse but this was after building up VERY SLOWLY, it is vital you pace and follow the guidelines to avoid flaring up. Once you are able to do a few minutes every day, you will find that there are great benefits.
If you grit your teeth and keep going through the pain, you will not only pay for it excruciatingly later but may also worsen the overall level of your day-to-day pain. Equally, if you keep stay in bed, keep still and do very little activity, you will also experience higher pain levels. Balancing rest and gentle movement is vital in managing pain.
Stress and Chronic Pain
Everyone with chronic pain knows how much worse it is when emotions are running high or you are stressed or even if those around you are stressed. It is a little like our bodies pick up these signals and translate everything into pain. The stress or adrenalin response is normally there to help us, flight, fight or freeze for example.
However, in chronic pain patients instead of enabling us to protect ourselves in response to danger, the stress can make our pain and other symptoms far worse causing a ‘wind up’ of the pain and opening of the pain gates.
Chronic pain itself is also a source of stress, which perpetuates the vicious cycle. Stressful thoughts about the pain and all the effect on our lives also magnify this effect and increase tension, which of course increases pain. Relaxation is even more important for those who live in pain. It can help reduce mental stress and also reduce physical muscle tension and the vicious cycle of ‘wind up’ broken.
Learn Relaxation Techniques
Relaxation is even more important when you live with chronic pain. Click here for some useful relaxation techniques to help you cope and your pain reduce.
For more advice on this and other aspects of flare-ups of pain, see Coping With Flare-ups of Pain.
This Self Care for Persistent Pain Toolkit video is definitely worth watching if you or your loved-ones suffer with chronic pain conditions view it here.
Remember to be patient and talk kindly to yourself.
As I add more posts with pain management techniques, use the drop-down menus to find support, coping techniques and further posts on managing your pain. Wishing you strength and far better days x
Sign-up and receive a free flare-up toolkit and regular posts and tips on living – and coping – with severe pain and chronic illness ♥
[avatar user=”jomalby” size=”thumbnail” link=”www.princessinthetower.org” target=”_blank”] Gentle hugs x[/avatar]