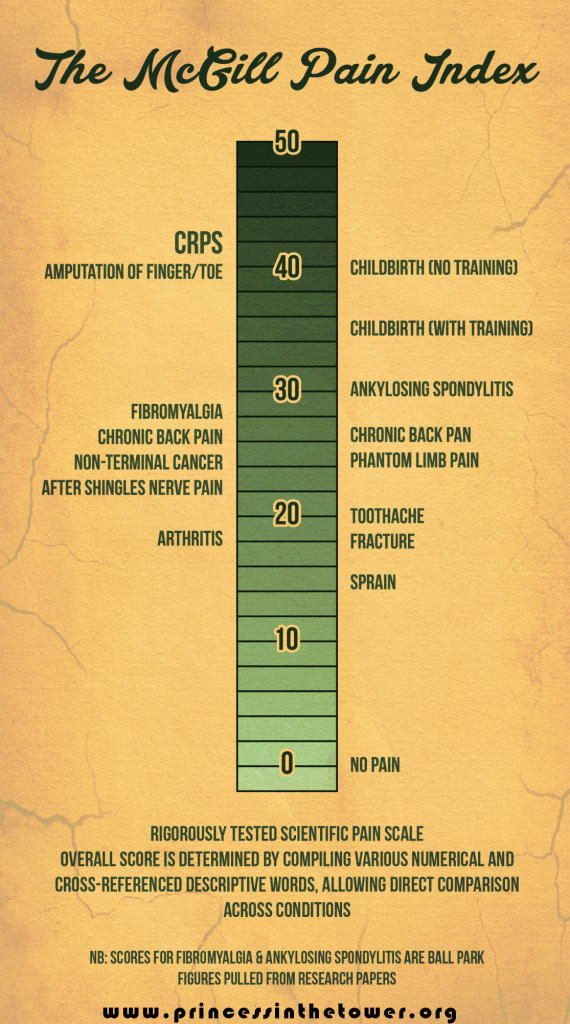
Complex Regional Pain Syndrome (CRPS), or Reflex Sympathetic Dystrophy (RSD), as it was previously known, is an excruciating chronic, and complex multi-system disease of the autonomic nervous system (dysautonomia), and central nervous system (CNS). CRPS causes constant pain that is recorded as being as severe as finger amputation without anaesthetic.
It is devastating for patients as is often diagnosed too late for full remission, though it is vital to never give up hope, people can and do go into remissions but sadly [at the moment] it is only a small percentage. However, with more research being done into this complex condition, our knowledge of CRPS is evolving and hopefully, we too as patients may benefit from that research.
For ways manage and treat CRPS: How to Manage and Treat Complex Regional Pain Syndrome; also see this open letter to those without CRPS.
CRPS is currently considered to be a multi-system condition that includes interactions between the immune system, the Autonomic Nervous System (ANS) and the Central Nervous System (CNS). There are a huge number of coexisting symptoms (see below), many of which are incredibly hard to deal with, particularly as they are so contrary to both how we appear (often looking healthy), and how at odds they are to ‘normal’ healthy human behaviour, as well as, our own response to life in constant pain.
When you’ve live in pain for many years, how you respond to that pain is vastly different from a healthy person. Equally, strange symptoms such as allodynic pain further complicate understanding, as well as our own ability to live with CRPS/RSD. Sounds, vibrations, hectic environments, or ones where many people are creating a lot of stimuli which then translates into excruciating, debilitating pain is another example of CRPS being so contrary, and hard to live with.
Living in a Painful World
“Sounds, especially loud or deep sounds and vibrations, will also cause pain; a school bell, thunder, loud music, crowds, singing, yelling, sirens, traffic, kids screaming, loud wind, even the sound in a typical movie theatre. This is what allodynia is all about,” says Keith Orsini from American RSDHope.
“Imagine going through your daily life where everything that you touch, or that touches you, where most every noise around you from a passing car or plane to children playing, causes you pain. In addition to the enormous pain you are already experiencing from the CRPS itself. Imagine living with that pain and allodynia 24 hours a day, every day, for months, years, and longer. There are many other symptoms but [pain and allodynia] are the two main ones that most patients talk about the most.”
Just as our CNS, ANS, and autoimmune systems act in perplexing, and painful ways, we too can find ourselves feeling equally perplexed, as aside from this complex cornucopia of symptoms, disability, and pain there’s no certainty. We can no more say how severe the pain will be 5 minutes from now than we can a week or a day, and this too creates further difficulties.
Everything from how we interact with loved-ones or day-to-day life, to the inability to attend so many ‘normal’ events for the duration, hectic and pain-inducing environments, and of course, the ignorance on the condition itself, all make living with this condition even more challenging.
Telling someone that they need to step back because the allodynic pain caused by them standing too close to you is making your nerves go crazy, or asking someone to speak more quietly or stop rustling a plastic bag all sound very strange yet these things can cause our already excruciating pain to crescendo, and magnifying our symptoms, and discomfort too.
Definitions of CRPS
CRPS is a severely disabling condition characterised by burning pain, increased sensitivity to all stimuli, and sensations of pain in response to normally non-painful stimuli including: light touch, a breeze, sound, vibration, bright lights and more. (Birklein et al., 2000; Wasner et al., 2003).
In addition, CRPS is characterised by motor disturbances such as weakness, tremor and muscle spasms (Veldman et al., 1993), and sympathetic dysfunction, such as changes in vascular tone, temperature changes and increased sweating (Birklein et al., 1998; Wasner et al., 2001).
Neurological effects of CRPS, including long term cognitive and mood changes (Marinus, J. et al, (2011) in ‘Clinical Features and Pathophysiology of Complex Regional Pain Syndrome’, The Lancet Neurology’, Vol 10, Issue 7, pp637-648) may be incorrectly treated as existing seaparetly from the condition, however new research will hopefully help raise awareness.
It has been shown that neuropsychological deficits are present in 65% of CRPS patients, including deficits in the executive functions, for example planning, organising, self-awareness, self-regulation and initiation of action, word recall lexical memory and conscious memory of events declarative memory.
Complex Regional Pain Syndrome (CRPS) involves neuropathic pain, glial cell activation leading to increased cytokines and ultimately central sensitization in the central nervous system, leading to centralised, body-wide chronic pain.
Sleep is massively affected, though this is unsurprising given the CNS and ANS changes and of course, constant severe pain (Schwartzman, R.J., et al. (2009) in ‘The Natural History of Complex Regional Pain Syndrome’, Clinical Journal of Pain, Vol. 25, Issue 4, pp. 273-280).
Another paper by Schwartzman, R.J. (2012) ‘Systemic complications of complex regional pain syndrome’ explains full body involvement and is a good one to print out if you are faced with what appears to be extensive spreading of our CRPS or many additional symptoms that cannot be otherwise explained. Robert Schwartzman is one of the leading experts in CRPS so this is definitely worth a read for both you and your doctor.
CRPS is currently viewed as involving interactions between the immune system, the ANS and the Central Nervous System (Rooij, A.M., (2010) in ‘Genetic and Epidemiological Aspects of Complex Regional Pain Syndrome’, Doctoral Thesis, Leiden University (ignore chapter 4 as it’s now been shown that their are no psychological differences between control groups & CRPS groups.
In most cases an upper or lower limb is affected but spreading can and does occur to other body parts, or many different body parts at the same time (as with full body or systemic CRPS) anywhere there are nerves can be involved (Stanton-Hicks et al., 1995) including internal organs.
Complex Regional Pain Syndrome (CRPS), formerly known as Reflex Sympathetic Dystrophy (RSD) is a neuroinflammatory condition that is characterized by a combination of sensory, autonomic, vasomotor, and motors dysfunctions. According to Bruehl and Chung (2006), CRPS may be understood as a biopsychosocial disorder, whereby psychological, behavioural and pathophysiological factors interact in a highly complex manner.
Most studies of CRPS have focused on the peripheral and spinal mechanisms responsible for the origin and development of the syndrome but the emerging view is that the peripheral (autonomic and somatosensory) changes in CRPS must be viewed as a manifestation of changes in the brain (Jänig and Baron,2002).
Echoing the brain and CNS involvement, I’ll quote directly from this more recent paper:
Complex regional pain syndrome is a disease of the central nervous system:
“CRPS patients exhibit changes which occur in somatosensory systems processing noxious, tactile and thermal information, in sympathetic systems innervating skin (blood vessels, sweat glands), and in the somatomotor system.
“This indicates that the central representations of these systems are changed and data show that CRPS is a systemic disease involving these neuronal systems. This way of looking at CRPS shifts the attention away from interpreting the syndrome conceptually in a narrow manner and to reduce it to one system or to one mechanism only, e.g., to sympathetic-afferent coupling.
“It will further our understanding why CRPS type I may develop after a trivial trauma, after a trauma being remote from the affected extremity exhibiting CRPS, and possibly after immobilisation of an extremity. It will explain why, in CRPS patients with sympathetically maintained pain, a few temporary blocks of the sympathetic innervation of the affected extremity sometimes lead to long-lasting (even permanent) pain relief and to resolution of the other changes observed in CRPS.
Another excruciating symptom is our inability to regulate temperature, the processing of tactile being unbearably painful, causing processing problems in thermal response, motor response, and vasomotor response, even leading to disturbed thermoregulatory reflexes and hypoesthesia on half or a quadrant of the body.
“The basis of extensive evidence from clinical observations and experimentation on humans, the hypothesis has been put forward that CRPS is a disease primarily of the central nervous system (CNS), involving changes in central sympathetic, somatosensory, and motor systems.
For example, Wasner et al 12 have shown that thermoregulatory reflexes are disturbed in the distal parts of the affected extremity in patients with CRPS I, which has been attributed to central changes reflected by alterations in the activity in cutaneous vasoconstrictor neurons.
Rommel et al 13,14 have demonstrated that up to 50% of patients with chronic CRPS I develop hypoesthesia on the entire half of the body or in the upper quadrant ipsilateral to the affected limb.
The anatomic distribution of these changes suggests that they might be due to changes in central processing of tactile stimuli, presumably at a thalamic or cortical level.
Additionally, in many patients, motor symptoms occur, including muscle weakness, tremor, dystonia, and a neglectlike syndrome. 15,16 These motor changes are unlikely to be related to a peripheral process but are supposed to be the result of specific alterations of the central motor system induced by the disease.1,11,17,18
Source: Functional Imaging of Central Nervous System Involvement in Complex Regional Pain Syndrome
To help prevent CRPS ALWAYS TAKE 1000mg/day VITAMIN C AFTER ANY SPRAIN OR STRAIN – this research shows that it can help to prevent CRPS from occurring.
Complex Regional Pain Syndrome is a multi-system disorder with clinical features of neurogenic inflammation, nociceptive sensitisation (which causes extreme sensitivity or allodynia), vasomotor dysfunction, and maladaptive neuroplasticity, generated by an aberrant response to tissue injury.
“CRPS is ranked as the highest form of chronic pain that exists in medical science today”
Reading 42 on the McGill Pain Scale (RSD/CRPS is referred to as Causalgia, which is Latin for “burning pain”). CRPS is a debilitating disease if not treated promptly and properly. The onset of CRPS usually follows a trauma, injury or surgery and increasing evidence suggests that psychological trauma can cause CRPS or increase the chance of its development after an injury by an estimated eight times.
See this post for ways manage and treat CRPS, while this is an open letter to those without CRPS. Without going into a full description of the disease, let us initially concentrate on the four main symptoms:
Constant chronic burning pain — also throbbing, aching stabbing, sharp, tingling, and/or crushing in the affected area or areas. Allodynia is a huge problem with RSD/CRPS (extreme pain response from innocuous stimuli); even a light breeze can cause pain, let alone the noise, lights, crowds and vibrations, all having a debilitating and life-limiting effect. In CRPS normal inputs such as touch, stroking and movement are misinterpreted as painful. This ongoing “painful” interpretation is a big part of the problem.
Inflammation — is not always present. It can take various forms, the skin may appear mottled, become easily bruised, have a shiny, dry, red, and tight look to it. An increase in sweating usually occurs as well.
Spasms in blood vessels and muscles of the extremities — this results in a feeling of coldness in the affected extremity, which feels like ice between the bones or fire burning the affected areas. Because of an inability to regulate our inner thermostats, touching something cool can be excruciating or cause freezing or burning pains. It depends on how long the CRPS has been present, and whether it is typically ‘hot’ CRPS or ‘cold’ CRPS.
This is as well as body fatigue, skin rashes, occasional low-grade fever and sore throats; swelling (edema), sores, dystonia, and tremors. The spasms can be confined to one area or be rolling in nature, moving up and down the leg, arm, or back.
Insomnia/Emotional Disturbance – CRPS affects the limbic system of the brain. This causes many problems that might not initially be linked to a disease like CRPS, among them are depression, insomnia, extreme difficulty concentrating, and short-term memory problems. Cognitive difficulties similar to fibro-fog are prevalent, simply due to the sensory overload of constant severe pain.
CRPS involves a malfunction of the nervous system that causes pain (often diffuse, intense and unrelenting) and related sensory abnormalities). Dysautonomia means dysregulation of the autonomic nervous system (ANS). The ANS controls involuntary bodily synergies between the sympathetic and parasympathetic nervous symptoms.
Necessary involuntary functions include things like heartbeat, breathing, digestion, and body temperature regulation. Studies have also linked the nervous system to the immune system, suggesting a possible correlation between ANS and autoimmune disorders.
In dysautonomia, the ANS does not respond to stimuli appropriately, either the parasympathetic or sympathetic nervous system can be hyporesponsive or hyperresponsive, often heightened by physiologic and psychologic stress. In those with mitochondrial dysautonomia, mitochondrial dysfunction is believed to cause the dysautonomia.
Since mitochondria provides a source of energy for cells, fatigue related diseases are common among mitochondrial myopathies. Nerve cells in the brain and muscles require significant energy and are depleted with mitochondrial malfunction.
Abnormal regulation of body temperature in mitochondrial disease patients is common, resulting in either a lower or higher baseline body temperature or a distinct intolerance to heat or cold. There may also be abnormal blood flow and sweating in the affected areas, problems with movement of the muscles and changes in the structure of the tissues (‘trophic’ changes).
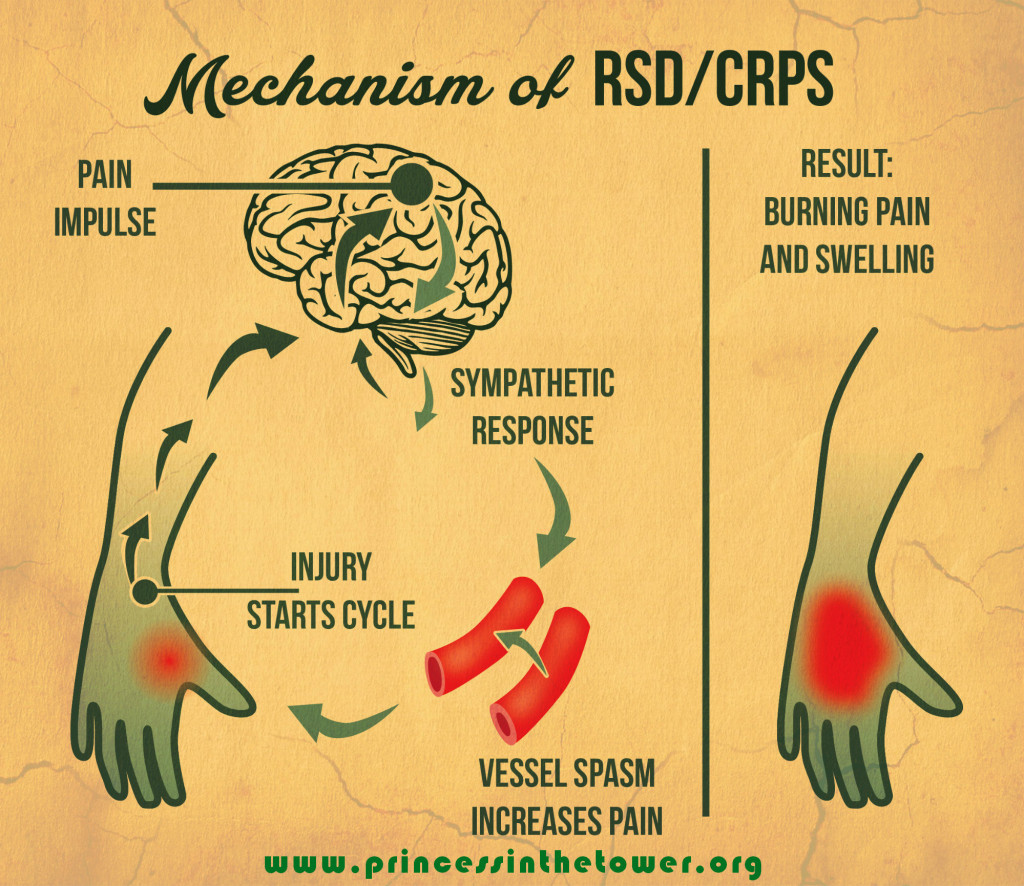
All of the above is now also attributed to the CNS involvement in CRPS/RSD. Complex Regional Pain Syndrome involves the skin, nerves, blood vessels, and bones. The sympathetic nervous system reacts to a stimulus, for example, an injury, although it could be as little as a spider’s bite. Blood flow may be affected in reaction to a burn, cut, or severe temperature changes. To stop you from using an injured limb, the limb swells. Sometimes inexplicably an abnormal or prolonged sympathetic reflex begins in a limb as reaction to a trauma.
The sympathetic nerves become overactive and can cause extensive symptoms that in turn cause debilitating consequences. There can be many symptoms but the most common one is severe, burning pain. Some of the other symptoms due to ANS dysfunction include swelling, temperature change, skin colour change, diminished motor function, and severe sweating.
These symptoms usually happen in a limb but can occur anywhere in the body, trunkel CRPS in the face or organs are some extreme examples. Symptoms may vary with each individual who has Complex Regional Pain Syndrome or CRPS/RSD.
Reflex Sympathetic Dystrophy (RSD)
Reflex Sympathetic Dystrophy/RSD is the former name for Complex Regional Pain Syndrome (CRPS). The name of Reflex Sympathetic Dystrophy (RSD) was changed to Complex Regional Pain Syndrome (CRPS) in 1993 by the International Association for the Study of Pain.
It has been known by many names such as algodystrophy or Causalgia or RSD, but is now most commonly known as CRPS. The are 2 forms of Complex Regional Pain Syndrome. The only difference between type 1 and type 2 is type two is easier to diagnose. CRPS type one is formerly known as RSD and CRPS type two was causalgia. Complex Regional Pain Syndrome and Reflex Sympathetic Dystrophy are used synonymously today.
Early Treatment
The main goal of treatment for CRPS is reversal of the course, amelioration of suffering, return to work if at all possible, avoiding surgical procedures such as amputation, and improvement in/some quality of life. The key to success is early diagnosis and early assertive treatment. Devastatingly, lack of proper understanding and proper diagnosis leads to improper treatment with poor outcome.
Read this post on: How to Manage and Treat Complex Regional Pain Syndrome for CRPS Awareness Month
There is a desperate need for future research in the treatment of CRPS
Delay in diagnosis is a factor in therapeutic failure. According to Poplawski, et al, treatment, and its results, are hampered by delay in diagnosis. Early diagnosis (up to 2 years) is essential for achieving the goal of successful treatment results. Simple monotherapy with only nerve block, only Gabapentin, or otherwise, is not sufficient for management of CRPS.
Treatment should be multidisciplinary and simultaneous: effective analgesia, proper antidepressants to reduce pain and insomnia; physiotherapy, nerve blocks, proper diet, when indicated channel blockers, and anticonvulsant therapy should be applied early and simultaneously. Administration of minimal treatments is apt to fail leading to lifelong disability and such severe pain that work is often seldom ever returned to.
Please raise awareness about Vitamin C:
To prevent getting CRPS/RSD ALWAYS TAKE 1000mg/day VITAMIN C AFTER ANY SPRAIN OR STRAIN Research shows that it can help to prevent CRPS/RSD from developing
RSD/CRPS Causes
-
– Trauma (physical trauma; there has also been evidence of psychological trauma causing a surge of activity in the amygdala and sympathetic nervous system/activation of glial cells, CRPS can occur in this instance when a secondary physical trauma happens simultaneously or while this activity is occurring)
-
– Soft-tissue injuries
-
– fractures heart disease (caused by inadequate blood supply)
-
– Spinal cord disorders
-
– Cerebral lesions
-
– Infections
-
– Surgery
-
– Repetitive motion disorder
-
– recent research suggests that severe emotional trauma prior to a physical trauma, massively increases the likelihood of CRPS developing
It is not known why these factors cause CRPS but there are many hypotheses that are the subject of research. Severe emotional trauma such as rape or abuse has been the suggested to increase the chances of CRPS developing, with so many patients being trauma survivors. Another interesting link made by a doctor at Bath Hospital was the correlation of eating disorders in the patient histories of those who have developed CRPS.
However, just as each human is unique, each case is unique. CRPS type two (causalgia) is defined by burning pain, allodynia (innocuous stimuli causing severe pain/an increase in symptoms), and onset usually occurs after nerve injury but it may be delayed.
The burning pain is constant and exacerbated by:

- – light
- – touch
- – vibration
- – stress
- – sounds
- – temperature
- – movement of the limb (though remaining still is also painful, it can be a strange art and balance)
- – emotional disturbance
- – someone standing to close or being very animated
- – barometric changes
Abnormalities in skin temperature and blood flow may occur as well as sudomotor dysfunction. Dystrophic changes may occur in the skin, hair or nails. CRPS vertigo and a whole host of ANS-disfunction symptoms may be experienced.
Pain
The pain of CRPS is constant and characterized, at least initially by burning—not in a descriptive sense but as if your limb or limbs are actually in a fire. This unrelenting pain intensifies with every movement or stimuls. Allodynia is involved (innocuous stimuli causing severe pain), making socialising even more complicated and painful. Even a light breeze is enough to make the pain rocket so having hectic people around massively increases the pain.
Inflammation
Swelling is sometimes localized, but often relentless in the initial stages of CRPS. Swelling intensifies the pain and promotes stiffness, which can be the beginning of atrophy and deformity.
Keeping the movement going is crucial—even if it is only wiggling your toes once every hour (and I know how excruciating this is but it can make the difference between dystrophy, atrophy, and dystonia, and maintaining mobility in the CRPS limb(s).
When tissue is injured or inflamed, excess fluid enters the tissues from damaged blood vessels within these tissues. If the veins cannot remove all of this fluid, it causes edema (swelling). Normally in healthy people, this swelling is temporary, and dissipates as tissues heal.
Swelling, and especially discolouration is one of the hallmark symptoms of CRPS early in the course of the disease where this inflammatory process causes edema. However, it is important to note that the huge delay in diagnosis means many patients are no longer presenting this symptom, and being misdiagnosed.
The swelling in CRPS may exist far longer than it would take normal tissue to heal because CRPS:
-
Prevents healing
-
Causes constant inflammation
-
May cause dilation of the arteries which will cause more fluid to leak, and may cause the veins to contract, which also prevent the normal removal of non-protein fluid from tissues.
-
The edema of CRPS/RSD may last for long periods of time
-
STIFFNESS, like swelling, is progressive resulting in less motion of the joints, which again, results in increased swelling and pain This in turn can produce further deformity and joint changes.
-
DISCOLOURATION indicates circulatory changes that diminish the nutrition of the tissues of the skin, ligaments, bones and tendons. The result is thin, shiny skin, pencil-like fingers and changes in ligaments. This further contributes to stiffness and pain. CRPS in the upper extremities had been classified in the following five ways, based on the location and intensity of symptoms.
Traditionally, complex regional pain syndrome was seen as a three-stage disease. However, these stages are increasingly being disregarded or seen as theoretical as all the features may or may not be present, with the speed of progression also varies hugely between patients.
Some patients never progress to stage III, others fluctuate, while others get to stage III and lose some of the symptoms of the earlier stages.
What is clear is the sooner you are diagnosed the better. Early recognition of the disease, correct diagnosis, and proper treatment, are all essential in keeping CRPS/RSD from becoming a chronic, life-long condition. Treatment must begin within months of onset, ideally within three months—which is why raising more awareness is so crucial to save others from this fate.
The following excerpt is taken from the America RSD Hope website:
1) The CONSTANT PAIN can be described as a burning pain. It feels as if a red hot poker were inserted into the affected area. it is also described as throbbing, aching stabbing, sharp, tingling, and/or crushing in the effected area; this is not always the site of the trauma. The effected area is usually hot or cold to the touch. The pain will be more severe than anticipated for the type of injury sustained. This is a hallmark of the disease.
Allodynia is typically present as well. Allodynia is an extreme sensitivity to touch, sound, vibration, barometric pressure changes, loud noises, wind/breeze, temperature, clothing, and even the gentle touch of a loved one.
This makes it increasingly difficult on the partners, children, and other loved ones, as their softest touch now causes pain instead of comfort. If a patient has not been diagnosed, and allodynia not properly explained, it can cause further distress to all involved, confusion, and doubt of the pain too. For more on “What Does CRPS Feel Like” click here.
2) INFLAMMATION is not always present in the same form but it can take various forms; the skin may appear mottled, become easily bruised, bleeding in the skin, small red dots, have a shiny, dry, red, and “tight” look to it. Increase in sweating usually occurs as well as swelling in and around the joints (shoulders, knees, wrists). In some patients a lack of sweating may occur, and some even go back and forth between the two.
3) The SPASMS result in a feeling of coldness in the effected extremity as well as body fatigue, skin rashes, low-grade fever, swelling (edema), sores, dystonia, and tremors. The spasms can be confined to one area or be rolling in nature; moving up and down the leg, arm, or back. They can involve not only muscles but also blood vessels.
4) The fourth part of this square is INSOMNIA and EMOTIONAL DISTURBANCE. CRPS affects the limbic system of the brain. Doctor Hooshang Hooshmand described it well:
“The fact that the sympathetic sensory nerve fibers carrying the sympathetic pain and impulse up to the brain terminate in the part of the brain called “limbic system”. This limbic (marginal) system which is positioned between the old brain (brainstem) and the new brain (cerebral hemispheres) is mainly located over the temporal and frontal lobes of the brain.”
This causes many problems that might not initially be linked to a disease like CRPS; chief among them are depression, insomnia and short-term memory problems but also includes agitation, irritability, and possibly even poor judgement.
CRPS can cause Depression, NOT the other way around. Read more here: RSD Hope – What is CRPS?
Here are some of the many symptoms of CRPS/RSD:
-
Skin temperature, skin colour changes
-
Pain caused by innocuous stimuli, for instance sound, vibration, light touch, even someone in the room can increase pain. Allodynia is pain from thing that you would never expect to cause pain, while hyperalgesia is an exaggerated pain response, so far more pain than should result from a stimulus.
-
Tremors, shakes, spasms and muscle contractions that can cause unusual movements and postures (dystonia)
-
Temperature changes and inability to regulate temperature
-
Changes in hair/nails/skin
-
Sweating changes, sometimes sweating varies from one side of the body to the other
-
Fluid build-up causing swelling (edema)
-
Lower bone density as they become more porous (osteoporosis)
-
Avoiding using the part of the body which hurts, which then causes additional problems like the muscles starting to waste away through lack of use (atrophy)
-
Central Nervous System (CNS) dysfunction and hyperactivity.
The CNS is made up of the brain and spinal cord which use the information from the wider spread ANS to control and co-ordinate what we do. The CNS can do strange things when it’s dependent on a faulty ANS for it’s information. As the condition develops the pain becomes continuous, it is truly relentless. There are brief periods where it may not be as severe, but considering that the pain experienced is off the scale of previous personal experience for most patients, the lesser pain moments are still excruciating by ‘normal’ standards. No wonder the natural response is to stop using whichever part of our body is affected.
Read more at: What is CRPS? | Elle and the Auto Gnome.
Complex regional pain syndrome in adults
Integrative conceptual model of CRPS. In the affected limb after trauma, enhanced anti-dromic secretion of neuropeptides from sensory nerve endings [77], enhanced release of immune mediators from various cells [22] and surface binding autoantibodies [54] may contribute both to change regional sensory nerve function, and elicit sensory axonal degeneration; resulting functional and structural changes may then elicit further changes creating a vicious cycle [70].
Some of these changes may be enhanced by tissue ischaemia ([59], data not shown). The long-lasting response of patients with long-standing CRPS to the—likely centrally acting—NMDA-receptor antagonist ketamine [47, 48] also suggests that, at least in chronic cases these regional factors do not sufficiently activate nociceptors (otherwise pain intensity would return as the ketamine plasma level declines); these factor may rather create a low-level activation of sensory nerves sustaining central sensitization in the dorsal horn (see main text).
Certain methods of brain training, and spinal cord stimulator treatment can, through yet unknown mechanisms alter regional factors in the affected limb, as evidenced by their reported efficacy to reduce limb swelling [13, 66, 92]. The model does not account for the presumed role of sympathetic dysfunction in some patients.
CRPS is a sympathetically mediated disorder
Sweating and colour/temperature differences between CRPS-affected and unaffected limbs are in part mediated by a complex sympathetic dysregulation. There is a low, rather than high, centrally mediated sympathetic outflow to cutaneous vasoconstrictors in the CRPS-affected extremity, which likely contributes to produce red and warm extremities [35]; other vasomotor signs such as cold temperature and bluish dyscolouration may be caused by reactive adrenoceptor up-regulation and/or supersensitivity, rather than by a dysregulation of the sympathetic outflow [36, 37].
Vaso- and sudomotor signs often diminish with time. The permanent cold temperature in some cases of late CRPS may be due to endothelial rather than sympathetic dysfunction [38]. Evans [39] had introduced the, now superseded term RSD to indicate that regional autonomic dysregulation actually causes the patients’ pain.
Hannington-Kiff [40] later suggested that agents that deplete the limb autonomic nerve endings of noradrenaline, such as regional guanethidine should, therefore, be effective. Unfortunately, all four RCTs conducted to assess this treatment have been negative [19]. Given the experience shared by many clinicians that this method, termed i.v. regional sympathetic block (IVRSB), actually does reduce pain in some patients, one wonders whether it is perhaps the application of tourniquet that conveys that effect. Indeed, IVRSB with saline may be more effective than IVRSB with guanethidine [41].
Local anaesthetic application to the sympathetic ganglia (i.e. stellate or lumbar sympathetic blocks) can relieve pain for the short term in selected patients [42], but repeat application does not prolong that effect [43]. Sympathetically maintained pain (SMP), that is pain that can be reduced by sympathetic blockade, although common in early CRPS, is rare in long-standing CRPS [44].
While there clearly is autonomic dysregulation [45], both the discussed rarity of SMP in those clinically particularly problematic long-standing cases, and the emergence of novel aetiological concepts have contributed to prompting CRPS experts to de-emphasize the importance of the concept of sympathetic dysfunction for advancing patient treatment.
Central sensitization is the driving factor for CRPS
Central sensitization is the molecular process that corresponds to the clinical observation that after a period of intense or repeated noxious stimulation (a noxious stimulus actually or potentially causes tissue damage), innocuous (non-noxious) stimuli become painful and remain painful (for a while at least) even if the initial noxious stimulation has subsided. This mechanism is important in most chronic pain [46].
Since N-methyl D-aspartate (NMDA) receptors play a critical role in central sensitization, the observation in two RCTs that low-dose i.v. ketamine (an NMDA antagonist) can dramatically reduce CRPS pain, indicates an important role for such central sensitization [47, 48].
There is currently no RCT evidence for high-dose ketamine coma under intensive care conditions, which has sometimes been discussed in the media [49]. In the two published low-dose RCTs, ketamine strongly reduced average pain intensity for several weeks independently of the CRPS disease duration, but without improving function. It is uncertain how these research findings will translate into clinical practice. Side effects from repeated ketamine infusions are poorly understood, and some experts have expressed concern about potential neurotoxicity [50].
Current protocols for ketamine treatment are expensive. In the published protocols, either a 5day hospital inpatient stay, or 10 consecutive working-day outpatient treatments are required to achieve pain relief lasting several weeks. Recently, a small pilot trial suggested efficacy of i.v. magnesium which, similar to ketamine, may work to reduce central sensitization [51].
Budapest diagnostic criteria (A–D must apply). Note that it is possible to distinguish between CRPS-1 (without damage to major nerves) and CRPS-2 [associated with (yet not causing) damage to a major nerve, a very rare presentation], but there is currently no RCT-derived evidence that this distinction has any consequence for treatment.
a. The reflected understanding of allodynia as painful sensation to a number of normally non-painful stimuli is under review by the IASP taxonomy group. Some experts suggest that the term allodynia should be reserved only for brush-stroke evoked pain (dynamic mechanical allodynia).
b. Hyperalgesia is exaggerated pain to a painful stimulus such as a pinprick.
c. For example, raised systemic inflammatory markers are not associated with CRPS, even in the initial inflammatory phase; such a finding of raised markers would lead to a search for an alternative or concomitant cause. Abnormal nerve conduction studies do not exclude CRPS, but the primary cause of the observed abnormality must be clarified: CRPS, by definition is always secondary, its presence cannot explain major nerve damage. Figure adapted from Ref. [4].
(Source: Complex regional pain syndrome in adults).
What Body Parts are Involved?
CRPS is a multi-symptom condition typically affecting one, two, or sometimes even all four extremities. It can also be in the face, shoulders, back, eyes, and other areas of the body as well. CRPS is an involvement of nerves, skin, muscles, blood vessels (causing constriction, spasms, and pain) as well as bones. This is from the Orthopod website:
Sympathetic nerves are responsible for conducting sensation signals to the spinal cord from the body. They also regulate blood vessels and sweat glands. Sympathetic ganglia are collections of these nerves near the spinal cord.
They contain approximately 20,000-30,000 nerve cell bodies. CRPS is felt to occur as the result of stimulation of sensory nerve fibers. Those regions of the body rich in nerve endings such as the fingers, hands, wrist, and ankles are most commonly affected.
When a nerve is excited, its endings release chemicals. These chemicals cause vasodilation (opening of the blood vessels). This allows fluid to leak from the blood vessel into the surrounding tissue. The result is inflammation or swelling leading to more stimulation of the sensory nerve fibers. This lowers the pain threshold. This entire process is called neurogenic inflammation.
This explains the swelling, redness, and warmth of the skin in the involved area initially. It also explains the increased sensitivity to pain. As the symptoms go untreated, the affected area can become cool, have hair loss, and have brittle or cracked nails. Muscle atrophy or shrinkage, loss of bone density (calcium), contracture, swelling, and limited range of motion in joints can also occur in the affected limb. These are in part caused by decreased blood supply to the affected tissues as the condition progresses.
(Source: A Patient’s Guide to Pain Management: Complex Regional Pain Syndrome)
Does RSD/CRPS Spread?
CRPS may spread from one part of the body to another regardless of where the original injury occurred. RSD/CRPS can spread in up to 70% of the cases. However, in an estimated number of cases (8% or less) it can become Systemic or body-wide. CRPS usually spreads up/down the same limb, or to the opposite limb but in an increasing number of cases it spreads to other areas of the body.
The pain of CRPS is continuous and it is widely recognised that it can be heightened by emotional or physical stress. Limbic system involvement suggests a propensity for trouble with sleeping, mood, appetite and sexual desire; in a study of 824 patients with CRPS, 92% reported insomnia, 78% irritability, agitation, anxiety, 73% depression and 48% had poor memory and felt they lacked concentration.
Patients are frequently classified into two groups based upon temperature, whether they are predominately “warm” or “hot” CRPS, or “cold” CRPS. The vast majority, approximately 70% of patients, have the “hot” type, which is said to be an acute form of CRPS. Cold CRPS is said to be indicative of a more chronic and long-term CRPS, affecting 30% of long-term CRPS patients.
With poorer McGill Pain Questionnaire (MPQ) scores, increased central nervous system involvement and a higher prevalence of dystonia, this new ‘stage’ (though the idea of stages of RSD/CRPS has been abandoned by pain specialists) of the CRPS can be managed but is obviously.
If you have developed Cold CRPS, trying to maintain mobility and keep movement in the area is vital. Microcirculation is compromised, though little is known – as with other CRPS cases – how to treat it. Obviously, heat therapy comes into its own here.
Prognosis is not favourable for cold CRPS patients, longitudinal studies suggest these patients have “poorer clinical pain outcomes and show persistent signs of central sensitisation correlating with disease progression.” The sympathetic nervous system is involved with CRPS, and as a form of dysautomnia, the autonomic nervous system can go haywire and cause a wide variety of strange symptoms.
Previously it was considered that CRPS had three stages; it is now believed that patients with CRPS do not progress through these stages sequentially. These stages may not be time-constrained, and could possibly be event-related, such as ground-level falls or re-injuries in previous areas.
CRPS Frustration
Complex Regional Pain Syndrome is frequently dismissed by health professionals for many reasons including:
-
They don’t understand the diagnosis and/or they are not familiar with the disorder.
-
They understand the diagnosis but lack experience in how to treat it properly.
-
Many think that the client is pretending to be ill or exaggerating their pain.
-
CRPS is thought to be hopeless and there is no cure (have hope!).
-
CRPS is purely psychological and that it is not a medical condition, i.e. “It’s all in your head”, which is clearly a myth.
-
Many people who work within the health care system dread accepting a client with CRPS because they know that effective treatment requires an ongoing, almost daily assessment of the condition to develop the proper regimen. It is far too time consuming for most clinics to adequately care for the patient. Generally, doctors like to cure not manage chronic illness.
-
Due to the nature of RSD/CRPS, the condition can quickly change for better or worse for reasons that are not fully understood. Therefore it is necessary to schedule evenly spaced treatment sessions in order to benefit, which is often not possible for many patients who now are unable to work.
-
The health care provider must address the plan of care very carefully once the diagnosis is made and must thoroughly customise therapy for each Complex Regional Pain Syndrome patient.
Many patients suffer needlessly through a lack of understanding from their GP/doctor, resulting in insufficient pain management that causes additional stress on an already over-taxed body. All individual characteristics (psychological, social, physiological) must be taken into account during therapy.
Communication between the family members, health professionals, and the patient must be clear, on-going and well established. It is common for the patient to have failed in a previous program if a positive, creative, caring relationship was not . If either the patient or the therapist senses a communication problem, it is far better to acknowledge that another clinician may be of greater benefit to the patient’s progress.
How is Complex Regional Pain Syndrome treated?
Everyone with CRPS needs good medical support and treatment. While this is not always possible, especially if you live in a rural or remote area, this website can help guide you in things that help improve your pain and function. Because pain involves the whole person, to get the best outcomes treatments and management usually require a combination of some of the following approaches:
- Pacing (also see Pain Management)
- Relaxation techniques; yoga; breathing; Tai Chi; Chi Kung etc.
- Mindfulness based relaxation
- Gentle movement and mobilisation techniques
- Coping and Managing your pain
- Use of pain medicines and medical procedures
- Brain-focused techniques
- Complimentary medicine (see Pain-Relief and Coping for Severe Pain)
The primary task is to eliminate or treat all possible causes. If there is no known cause, or if with the removal of the cause, the symptoms do not satisfactorily disappear, then there are only the symptoms of RSD/CRPS to be treated. Successful treatment of RSD/CRPS is dependent on:
- Early diagnosis. If diagnosed early, the prognosis is very good.
- Begin treatment of the underlying cause, if there is one. If not, then focus on the treatment of the RSD/CRPS process.
- The key approach is to provide adequate pain relief in order to undertake rehabilitation with the primary aim of restoring function as early as possible. Also, with the recent research in neuroscience, it is vital to control pain so that pain pathways in the brain do not become maladaptively rewired, making recovery even more difficult.
Scroll down for What You Can Do For Your CRPS (and the links and resources below). Also see: How to Manage and Treat Complex Regional Pain Syndrome.
CRPS: Advanced Concepts as Illustrated by Case Histories
Dr. Getson discusses complications and comorbidities associated with CRPS:
What Does CRPS/RSD Feel Like?
CRPS pain can be anywhere in the body where there are nerves. It has a fusion of excruciating qualities from pain much like holding your limbs in a fire, to a freezing burning pain (especially with ‘cold’ CRPS). There are also stabbing, shooting pains, ‘broken glass’ type pains, many patients use the metaphor of being ‘filled with bees’ as it never pauses, and is always instense.
CRPS presents most commonly in the four extremities but many have systemic CRPS, or ‘spreading’ in other areas, including less common areas, such as their eyes, ears, back, face. Here Keith Orsini from RSD Hope answers the question: what does it feel like?
“Well, if you had it in your hand, imagine your hand was doused in gasoline, lit on fire, and then kept that way 24 hours a day, 7 days a week, and you knew it was never going to be put out. Now imagine it both hands, arms, legs, feet; well, you get the picture. I sometimes sit there and am amazed that no one else can see the flames shooting off of my body. The second component to CRPS is what is called Allodynia.
“Allodynia is an extreme sensitivity to touch, sound, and/or vibration. Imagine that same hand now has the skin all burned off and is completely raw. Next, rub some salt on top of it and then rub some sandpaper on top of that! THAT is allodynia! Picture getting pretty vivid? Now, because of the allodynia, any normal touch will cause pain; your clothing, the gentle touch of a loved one, a sheet, rain, shower, razor, hairbrush, shoe, someone brushing by you in a crowded hallway, etc.
“In addition, sounds, especially loud or deep sounds and vibrations, will also cause pain; a school bell, thunder, loud music, crowds, singing, yelling, sirens, traffic, kids screaming, loud wind, even the sound in a typical movie theatre. This is what allodynia is all about.
“Imagine going through your daily life where everything that you touch, or that touches you, where most every noise around you from a passing car or plane to children playing, causes you pain. In addition to the enormous pain you are already experiencing from the CRPS itself. Imagine living with that pain and allodynia 24 hours a day, every day, for months, years, and longer. There are many other symptoms but these are the two main ones that most patients talk about the most,” says Keith Orsini.
What Does CRPS Feel Like? – American RSDHope.
What You Can Do For Your CRPS:
How to Manage and Treat Complex Regional Pain Syndrome
Pain education
To manage pain and gain more control over your life and symptoms in spite of CRPS, you must understand how pain behaves. Visit the Pain Management page for more info and watch a great video with the amazing Prof, Lorimer Moseley, who banishes the jargon and offers a description of the pain process that even the most unscientific of pain princesses can understand.
Mobilisation & massage techniques
For pain relief, to reduce stiffness, increase circulation, ease movement and gain a good sense of your body; all important in the recovery process but also if you need to spend a long time in bed or resting due to high pain levels. see Pain-Relief and Coping for Severe Pain.
Specific exercises
To mobilise tight & stiff body regions, to develop normal control of movement; gradually progressing from just a couple of repetitions to ten (see a physiotherapist for guidance on how to strengthen disused muscles).
General exercise
To progressively build up your tolerance and confidence for daily activity and your chosen exercises; always keep within your limitations, increasing your timed activity very gradually. Read this blog post on Therapeutic Yoga with a restorative yoga sequence, which can be very healing and gentle enough to not cause a flare-up of symptoms; swimming/aqua physio is immensely helpful with RSD/CRPS.
Graded exposure & pacing
There are often particular activities that are challenging, painful and sometimes avoided for fear of causing damage or harm. With new knowledge of pain and confidence to move you can gradually re-engage with some of these activities. Pacing means that you set a baseline and work towards your goals, see the Pain Management page for more information.
Brain-Focused Strategies
Modern neuroscience has delivered us new ways of approaching pain though our understanding of the brain when we are in pain, in particular chronic or persisting pain. We can target the adaptations and changes that have been found via particular types of sensory and motor training. For example graded motor imagery.
Mindfulness & focused attention training
To gain control over your attention and emotional regulation; there has been a spotlight placed upon these techniques in recent years due to their effectiveness in stress and pain. We teach and practice mindfulness and other cognitive methods as a way of reducing the emotional aspects of pain, to directly tackle stress and to optimise performance. Click here for an example of one of the mindfulness techniques.
Imagery & visualisation
Motor imagery is used as part of the graded motor imagery programme and as a stand alone brain focused training. When we think about movement, the same areas of the brain are active as when we actually move. Using this physiology within the cortical network allows us to re-train normal movement (how the brain plans and then executes precise and well controlled actions) at the early stages of rehabilitation. Visualisation is a way of changing the body physiology in a positive manner thereby benefiting the physical self, mood and creating a positive context for rehabilitation.
When it All Gets Too Much
The suicide rate among RSD/CRPS sufferers is extremely high due to the intensity of the never-ending pain, sleep deprivation, frustration, social isolation, misunderstanding, and lack of support from medical professionals, family and friends. If you are a patient suffering from depression and contemplating suicide, please, please get help – Suicide Prevention / Depression Support:
· UK: Samaritans (National and local): 08457 90 90 90 or jo@samaritans.org
· UK: Painline: 0845 603 1593
· Pain Association Scotland: 0800 783 6059
· Pain Concern UK: 01620 822 572
· US: Hopeline (Suicide Prevention): 1-800-SUICIDE (1-800-784-2433)
· US: Suicide Hotline: 1-800-273-Talk (1-800-8255)
· US: Directory of Local Helplines / Centers
· Global: Befrienders Worldwide Directory of Suicide Hotlines
Feeling suicidal is not a character defect, and it doesn’t mean that you are crazy, or weak, or flawed. It only means that you have more pain than you can cope with right now. Please read this fantastic guide before you do anything that will leave everyone wondering if there was something that they could do. No matter how you feel in this moment, and no matter how impossible it may seem, things can and do improve.
Life with severe, constant pain is hard, very hard. There will be times when what is already excruciating flares up to being beyond comprehension in terms of pain (I know I’m often astonished at just how limitless the variety and intensity of pain can be), and it is these times where you must take extra special care of yourself and mind. Read Techniques to Help Depression for help with depression. More will be added regularly.
Know that you’re not alone; the human mind can sometimes be your own worst enemy, especially when bottling up how you’re feeling both physically and mentally. Consider joining a community who knows how you’re feeling and speak with members who have first-hand experience with depression stemming from RSD/CRPS.
The Princess in the Tower Facebook page is another lovely space to meet others with RSD/CRPS and or other pain conditions. If you enjoy Twitter, follow @APainPrincess for regular posts and offerings.
Also see: How to Manage and Treat Complex Regional Pain Syndrome
“For those who understand no explanation is needed. For those who do not understand no explanation is possible.” ~ Rosemary Eagle, CRPS patient, advocate, and artist
Links, Resources & Downloads:
Complex Regional Pain Syndrome: Free pamphlet on CRPS from the National Health Institute.
Burning Nights CRPS — informative and regualrly updated info, highly recommended
CRPS UK 2012 Guidelines: These were released in 2012 — see RCP updated 2018 guidelines above — this document has plenty of info’ that may help you to educate your doctor, or any other practitioner.
“To provide guidance on the diagnosis, prevention and treatment of complex regional pain syndrome (CRPS) in adults, in a variety of clinical settings. The guideline addresses the diagnosis, prevention and treatment of adult patients with suspected or diagnosed CRPS in both primary and secondary care. The guideline is for use by all healthcare professionals involved in caring for patients with CRPS or suspected CRPS. This includes general practitioners, hospital doctors, nurses, physiotherapists, occupational therapists and psychologists in primary and secondary care.”
Just click on the option to download the guidelines PDF and it will open the document for you to save it to your computer and/or print it off.
Complex Regional Pain Syndrome: Diagnosis and Management — Dr. Chopra — Download pdf here
Inspired & Informative CRPS Blogs
Although ever in the process of adding more, these blogs and resources are from truly wonderful friends and fellow advocates living with CRPS (their sites are rich with info quite unmatched online). Sign-up or follow and enjoy offerings so heady with both care and content, I may even lose you for good:
Burning Nights CRPS — informative and regualrly updated info, highly recommended
Biowizardry: Cauterizing the Bleeding Edge — Biowizardry combines CRPS info and experience created by scientist and CRPS patient—very interesting blog!
RSDCRPS Research and Developments Facebook Page
Doesn’t Own Me – There are millions of people, but only one YOU. Don’t let pain change that!
The Invisible Warrior – CRPS Chronicles
RSD/CRPS Research and Developments, an unbiased research page
CRPS Frequently Asked Questions: “So you’ve been diagnosed with RSD and/or CRPS… What now?”
Also see Elle and the Autognome’s wonderful page, especially for the dysautomnia info, which is hard to find: Elle and the Auto Gnome (Living with RSD / CRPS & Dysautonomia)
SPOONIE SERIES – Laura Spoonie Blogs — One Spoon at a Time
Taming of the Beast is the Facebook page for the website mentioned above and also a resource for natural healing and alternative health:
November is CRPS Awareness Month
Also, feel free to add your blog or favourite suggestions in the Guest Book as I am updating everything as often as princessly possible.
Sign-up and receive a free flare-up toolkit and the occasional newsletter with tips on living — and coping — with severe pain and chronic illness ♥
[avatar user=”jomalby” size=”thumbnail” link=”www.princessinthetower.org” target=”_blank”] Gentle hugs x[/avatar]
[This page is updated as regularly as possible]